Skin of Colour Resource
Hyperpigmentation (see also Melasma)
Hyperpigmentation—general

Melanonychia. © DermNetNZ
Natural Cosmeceutical Ingredients for the Management of Hyperpigmentation in Hispanic and Latino Women. Murphy MJ, Dow AA. J Clin Aesthet Dermatol. 2021 Aug;14(8):52-56. Epub 2021 Aug 1. PMID: 34840659; PMCID: PMC8570660. Review.
A Review of Oral Therapies for the Treatment of Skin Hyperpigmentation. Shimshak SJE, Tolaymat LM, Haga CB, Dawson NL, Gillis MS, Yin M, Kirsch B, Cooper M, Sluzevich JC. J Cutan Med Surg. 2022 Mar-Apr;26(2):169-175. doi: 10.1177/12034754211045391. Epub 2021 Sep 19. PMID: 34541912. Review.
Applications of microneedling for various dermatologic indications with a special focus on pigmentary disorders: A comprehensive review study. Ziaeifar E, Ziaeifar F, Mozafarpoor S, Goodarzi A. Dermatol Ther. 2021 Oct 17:e15159. doi: 10.1111/dth.15159. Online ahead of print. PMID: 34657363 Review.
Dermoscopy of acquired pigmentary disorders: a comprehensive review. Krueger L, Saizan A, Stein JA, Elbuluk N. Int J Dermatol. 2021 Jul 7. doi: 10.1111/ijd.15741. Online ahead of print. PMID: 34235719 Review.
Modulating skin colour: role of the thioredoxin and glutathione systems in regulating melanogenesis. Lu Y, Tonissen KF, Di Trapani G. Biosci Rep. 2021 Apr 19:BSR20210427. doi: 10.1042/BSR20210427. Online ahead of print. PMID: 33871027
Periorbital Discolouration Diagnosis and Treatment: Evidence-Based Review. Pissaridou MK, Ghanem A, Lowe N. J Cosmet Laser Ther. 2020 Nov 16;22(6-8):217-225. doi: 10.1080/14764172.2021.1899238. Epub 2021 Jun 3. PMID: 34078228 Review.
Emerging topical therapies to treat pigmentary disorders: an evidence-based approach. Hu S, Laughter MR, Anderson JB, Sadeghpour M. J Dermatolog Treat. 2021 Jun 23:1-7. doi: 10.1080/09546634.2021.1940811. Online ahead of print. PMID: 34114938
Post-Inflammatory Hyperpigmentation: A Review of Treatment Strategies. Shenoy A, Madan R. J Drugs Dermatol. 2020 Aug 1;19(8):763-768. doi: 10.36849/JDD.2020.4887. PMID: 32845587 Review.
A comprehensive review of the therapeutic potential of α-arbutin. Saeedi M, Khezri K, Seyed Zakaryaei A, Mohammadamini H. Phytother Res. 2021 Aug;35(8):4136-4154. doi: 10.1002/ptr.7076. Epub 2021 Mar 16. PMID: 33724594 Review.
Anti-Pigmentary Natural Compounds and Their Mode of Action. Kim K, Huh Y, Lim KM. Int J Mol Sci. 2021 Jun 8;22(12):6206. doi: 10.3390/ijms22126206. PMID: 34201391 Free PMC article. Review.
Topical treatment for postinflammatory hyperpigmentation: a systematic review. Tan MG, Kim WB, Jo CE, Nabieva K, Kirshen C, Ortiz AE. J Dermatolog Treat. 2021 Sep 27:1-9. doi: 10.1080/09546634.2021.1981814. Online ahead of print. PMID: 34525885
Topical treatment strategies to manipulate human skin pigmentation. Rachmin I, Ostrowski SM, Weng QY, Fisher DE. Adv Drug Deliv Rev. 2020 Jan 1;153:65-71. doi: 10.1016/j.addr.2020.02.002. Epub 2020 Feb 21. PMID: 32092380 Free PMC article.
Dermoscopy of acquired pigmentary disorders: a comprehensive review. Krueger L, Saizan A, Stein JA, Elbuluk N. Int J Dermatol. 2021 Jul 7. doi: 10.1111/ijd.15741. Online ahead of print. PMID: 34235719 Review.
A Review of Oral Therapies for the Treatment of Skin Hyperpigmentation. Shimshak SJE, Tolaymat LM, Haga CB, Dawson NL, Gillis MS, Yin M, Kirsch B, Cooper M, Sluzevich JC. J Cutan Med Surg. 2021 Sep 19:12034754211045391. doi: 10.1177/12034754211045391. Online ahead of print. PMID: 34541912
Anti-Pigmentary Natural Compounds and Their Mode of Action. Kim K, Huh Y, Lim KM. Int J Mol Sci. 2021 Jun 8;22(12):6206. doi: 10.3390/ijms22126206. PMID: 34201391 Free PMC article. Review.
Role of Amine Neurotransmitters and Their Receptors in Skin Pigmentation: Therapeutic Implication. Enkhtaivan E, Lee CH. Int J Mol Sci. 2021 Jul 28;22(15):8071. doi: 10.3390/ijms22158071. PMID: 34360837 Free PMC article. Review.
A comprehensive review of the therapeutic potential of α-arbutin. Saeedi M, Khezri K, Seyed Zakaryaei A, Mohammadamini H. Phytother Res. 2021 Aug;35(8):4136-4154. doi: 10.1002/ptr.7076. Epub 2021 Mar 16. PMID: 33724594 Review.
Emerging topical therapies to treat pigmentary disorders: an evidence-based approach. Hu S, Laughter MR, Anderson JB, Sadeghpour M. J Dermatolog Treat. 2021 Jun 23:1-7. doi: 10.1080/09546634.2021.1940811. Online ahead of print. PMID: 34114938
Modulating skin colour: role of the thioredoxin and glutathione systems in regulating melanogenesis. Lu Y, Tonissen KF, Di Trapani G. Biosci Rep. 2021 Apr 19:BSR20210427. doi: 10.1042/BSR20210427. Online ahead of print. PMID: 33871027
The effect of Vitamin C on melanin pigmentation - A systematic review.
Sanadi RM, Deshmukh RS.
J Oral Maxillofac Pathol. 2020 May-Aug;24(2):374-382. doi: 10.4103/jomfp.JOMFP_207_20. Epub 2020 Sep 9. Systematic review.
Therapeutic options for management of Hori's Nevus: A systematic review.
Kaur H, Sarma P, Kaur S, Kaur H, Prajapat M, Mahendiratta S, Kumar S, Thota P, Parsad D, Medhi B.
Dermatol Ther . 2019 Nov 12. doi: 10.1111/dth.13167. [Epub ahead of print]. Systematic review.
Erythema dyschromicum perstans: A case report and systematic review of histologic presentation and treatment.
Leung N, Oliveira M, Selim MA, McKinley-Grant L, Lesesky E.
Int J Womens Dermatol. 2018 Sep 27;4(4):216-222. doi: 10.1016/j.ijwd.2018.08.003. eCollection 2018 Dec. Systematic review.
Are natural ingredients effective in the management of hyperpigmentation? A systematic review.
Hollinger JC, Angra K, Halder RM.
J Clin Aesthet Dermatol. 2018 Feb;11(2):28-37. Epub 2018 Feb 1. Systematic review.
Pitfalls in clinical trials reveal need for well tolerated, more effective depigmenting agents.
Saxena S, Andersen RM, Maibach HI.
J Dermatolog Treat. 2015 Oct;26(5):440-50. doi: 10.3109/09546634.2014.998609. Epub 2015 Feb 11. Systematic review.
The use of botanically derived agents for hyperpigmentation: a systematic review.
Fisk WA, Agbai O, Lev-Tov HA, Sivamani RK.
J Am Acad Dermatol. 2014 Feb;70(2):352-65. doi: 10.1016/j.jaad.2013.09.048. Epub 2013 Nov 23. Systematic review.
The role of topical retinoids in the treatment of pigmentary disorders: an evidence-based review.
Kang HY, Valerio L, Bahadoran P, Ortonne JP.
Am J Clin Dermatol. 2009;10(4):251-60. doi: 10.2165/00128071-200910040-00005. Systematic review.
Inhibition of melanogenesis by some well-known polyphenolics: A review.
Orhan IE, Deniz FSS.
Curr Pharm Biotechnol. 2020 Dec 10. doi: 10.2174/1386207323666201211102233. Online ahead of print. Review.
[Topical treatment of pigmentation disorders with cosmetic and pharmaceutical agents].
Kerscher M, Buntrock H.
Hautarzt. 2020 Dec;71(12):944-949. doi: 10.1007/s00105-020-04719-8. German. Review.
[Chemical peeling for treatment of melasma, pigmentary disorders and hyperpigmentation : Indications, effectivity and risks].
Borelli C, Fischer S.
Hautarzt. 2020 Dec;71(12):950-959. doi: 10.1007/s00105-020-04712-1. German. Review.
[Laser treatment of pigmentation disorders].
Fritz K, Salavastru C.
Hautarzt. 2020 Dec;71(12):920-925. doi: 10.1007/s00105-020-04716-x. German. Review.
The top ten cosmeceuticals for facial hyperpigmentation.
Searle T, Al-Niaimi F, Ali FR.
Dermatol Ther. 2020 Jul 27:e14095. doi: 10.1111/dth.14095. Online ahead of print. Review.
The use of botanical extracts in East Asia for treatment of hyperpigmentation: An evidenced-based review.
Hu S, Wolfe S, Laughter MR, Sadeghpour M.
J Drugs Dermatol. 2020 Jul 1;19(7):758-763. doi: 10.36849/JDD.2020.4776. Review.
Emulsified fat and nanofat for the treatment of dark circles.
Ziade G, Karam D.
Dermatol Ther. 2020 Jul 28:e14100. doi: 10.1111/dth.14100. Online ahead of print. Review.
Emerging role of dermal compartment in skin pigmentation: Comprehensive review.
Kapoor R, Dhatwalia SK, Kumar R, Rani S, Parsad D.
J Eur Acad Dermatol Venereol. 2020 Apr 3. doi: 10.1111/jdv.16404. [Epub ahead of print]. Review.
Cutaneous interaction with visible light: What do we know.
Cohen L, Brodsky MA, Zubair R, Kohli I, Hamzavi IH, Sadeghpour M.
J Am Acad Dermatol. 2020 Apr 11. pii: S0190-9622(20)30551-X. doi: 10.1016/j.jaad.2020.03.115. [Epub ahead of print]. Review.
Melanogenic difference consideration in ethnic skin type: A balance approach between skin brightening applications and beneficial sun exposure.
Markiewicz E, Idowu OC.
Clin Cosmet Investig Dermatol. 2020 Mar 9;13:215-232. doi: 10.2147/CCID.S245043. eCollection 2020. Review.
Topical treatment strategies to manipulate human skin pigmentation.
Rachmin I, Ostrowski SM, Weng QY, Fisher DE.
Adv Drug Deliv Rev. 2020 Feb 21. pii: S0169-409X(20)30008-9. doi: 10.1016/j.addr.2020.02.002. [Epub ahead of print]. Review.
Therapeutic insights in melasma and hyperpigmentation management.
Huerth KA, Hassan S, Callender VD.
J Drugs Dermatol. 2019 Aug 1;18(8):718-729. Review.
Ashy dermatosis: a review.
Nguyen K, Khachemoune A.
Dermatol Online J. 2019 May 15;25(5). pii: 13030/qt44f462s8. Review.
What's new in pigmentary disorders.
Zubair R, Lyons AB, Vellaichamy G, Peacock A, Hamzavi I.
Dermatol Clin. 2019 Apr;37(2):175-181. doi: 10.1016/j.det.2018.12.008. Epub 2019 Feb 16. Review.
Hyperpigmentation disorders in Hispanic population in the United States.
Rendon MI.
J Drugs Dermatol. 2019 Mar 1;18(3):s112-114. Review.
Dyschromatosis symmetrica hereditaria and reticulate acropigmentation of Kitamura: An update.
Kono M, Akiyama M.
J Dermatol Sci. 2019 Jan 15. pii: S0923-1811(19)30005-2. doi: 10.1016/j.jdermsci.2019.01.004. [Epub ahead of print]. Review.
Dermoscopy of pigmentary disorders in brown skin.
Chatterjee M, Neema S.
Dermatol Clin. 2018 Oct;36(4):473-485. doi: 10.1016/j.det.2018.05.014. Review.
Melanogenesis inhibitors.
Kumari S, Thng STG, Verma NK, Gautam HK.
Acta Derm Venereol. 2018 Jul 4. doi: 10.2340/00015555-3002. [Epub ahead of print]. Review.
Inhibitors of melanogenesis: An updated review.
Pillaiyar T, Namasivayam V, Manickam M, Jung SH.
J Med Chem. 2018 May 24. doi: 10.1021/acs.jmedchem.7b00967. [Epub ahead of print]. Review.
Pigmentation disorders: Diagnosis and management.
Plensdorf S, Livieratos M, Dada N.
Am Fam Physician. 2017 Dec 15;96(12):797-804. Review.
Pigmented fungiform lingual papillae: dermoscopic and clinical features.
Chessa MA, Patrizi A, Sechi A, Virdi A, Leuzzi M, Neri I.
J Eur Acad Dermatol Venereol. 2018 Jan 22. doi: 10.1111/jdv.14809. [Epub ahead of print] Review.
Updated review of genetic reticulate pigmentary disorders.
Zhang J, Li M, Yao Z.
Br J Dermatol. 2017 Oct;177(4):945-959. doi: 10.1111/bjd.15575. Epub 2017 Sep 27. Review.
Pediatric disorders of pigmentation commonly seen in skin of color.
Ascha M, Irfan M.
Semin Cutan Med Surg. 2016 Dec;35(4):191-200. doi: 10.12788/j.sder.2016.064. Review.
Facial hyperpigmentation in skin of color: Special considerations and treatment.
Vashi NA, Wirya SA, Inyang M, Kundu RV.
Am J Clin Dermatol. 2016 Dec 9. [Epub ahead of print]. Review.
Facial hyperpigmentation in darker skin types: Part 2.
Bala HR, Rodrigues M.
Dermatology in Practice. 2016 Winter;22(4):105-108. Review.
Skin hyperpigmentation in Indian population: Insights and best practice.
Nouveau S, Agrawal D, Kohli M, Bernerd F, Misra N, Nayak CS.Indian J Dermatol. 2016 Sep-Oct;61(5):487-95. doi: 10.4103/0019-5154.190103. Review.
Lichen planus pigmentosus: The controversial consensus.
Ghosh A, Coondoo A.
Indian J Dermatol. 2016 Sep-Oct;61(5):482-6. doi: 10.4103/0019-5154.190108. Review.
Facial hyperpigmentation in darker skin types: Part 1.
Bala HR, Rodrigues M.
Dermatology in Practice. 2016 Autumn;22(3):79-82. Review.
Hyperpigmentation therapy: a review.
Desai SR.
J Clin Aesthet Dermatol. 2014 Aug;7(8):13-7. Review.
What's new in objective assessment and treatment of facial hyperpigmentation?
Molinar VE, Taylor SC, Pandya AG.
Dermatol Clin. 2014 Apr;32(2):123-35. doi: 10.1016/j.det.2013.12.008. Review.
New and emerging treatments for hyperpigmentation.
Alexis AF.
J Drugs Dermatol. 2014 Apr;13(4):382-5. Review.
Polypodium leucotomos as an adjunct treatment of pigmentary disorders.
Nestor M, Bucay V, Callender V, Cohen JL, Sadick N, Waldorf H.
J Clin Aesthet Dermatol. 2014 Mar;7(3):13-7. Review.
Acquired hyperpigmentations.
Cestari TF, Dantas LP, Boza JC.
An Bras Dermatol. 2014 Jan-Feb;89(1):11-25. doi: 10.1590/abd1806-4841.20142353. Review.
Pigmentation disorders: hyperpigmentation and hypopigmentation.
Nicolaidou E, Katsambas AD.
Clin Dermatol. 2014 Jan-Feb;32(1):66-72. doi: 10.1016/j.clindermatol.2013.05.026. Review.
Facial hyperpigmentation: causes and treatment.
Vashi NA, Kundu RV.
Br J Dermatol. 2013 Oct;169 Suppl 3:41-56. doi: 10.1111/bjd.12536. Review.
Clinicopathological correlation of acquired hyperpigmentary disorders.
Patel AB, Kubba R, Kubba A.
Indian J Dermatol Venereol Leprol. 2013 May-Jun;79(3):367-75. doi: 10.4103/0378-6323.110798. Review.
Retinoids and azelaic acid to treat acne and hyperpigmentation in skin of color.
Woolery-Lloyd HC, Keri J, Doig S.
J Drugs Dermatol. 2013 Apr;12(4):434-7. Review.
Dermocosmetic management of hyperpigmentations.
Guerrero D.
Ann Dermatol Venereol. 2012 Dec;139 Suppl 4:S166-9. doi: 10.1016/S0151-9638(12)70130-8. Review.
New horizons in treating disorders of hyperpigmentation in skin of color.
Konda S, Geria AN, Halder RM.
Semin Cutan Med Surg. 2012 Jun;31(2):133-9. doi: 10.1016/j.sder.2012.03.001. Review.
Treatment of hyperpigmentation.
Woolery-Lloyd H, Kammer JN.
Semin Cutan Med Surg. 2011 Sep;30(3):171-5. doi: 10.1016/j.sder.2011.06.004. Review.
Topical retinoids for pigmented skin.
Geria AN, Lawson CN, Halder RM.
J Drugs Dermatol. 2011 May;10(5):483-9. Review.
Management of hyperpigmentation in darker racial ethnic groups.
Grimes PE.
Semin Cutan Med Surg. 2009 Jun;28(2):77-85. doi: 10.1016/j.sder.2009.04.001. Review.
Latest insights into skin hyperpigmentation.
Ortonne JP, Bissett DL.
J Investig Dermatol Symp Proc. 2008 Apr;13(1):10-4. doi: 10.1038/jidsymp.2008.7. Review.
New and experimental treatments of cloasma and other hypermelanoses.
Picardo M, Carrera M.
Dermatol Clin. 2007 Jul;25(3):353-62, ix. Review.
Utilizing combination therapy for ethnic skin.
Taylor SC.
Cutis. 2007 Jul;80(1 Suppl):15-20. Review.
Established treatments of skin hypermelanoses.
Nikolaou V, Stratigos AJ, Katsambas AD.
J Cosmet Dermatol. 2006 Dec;5(4):303-8. Review.
[Treatment of localised hyperpigmentation in black skin].
Sulimovic L.
Ann Dermatol Venereol. 2006 Nov;133(11):940-4. Review. French. No abstract available.
Retinoid therapy of pigmentary disorders.
Ortonne JP.
Dermatol Ther. 2006 Sep-Oct;19(5):280-8. Review.
Increasing our understanding of pigmentary disorders.
Grimes P, Nordlund JJ, Pandya AG, Taylor S, Rendon M, Ortonne JP.
J Am Acad Dermatol. 2006 May;54(5 Suppl 2):S255-61. Review.
Hyperpigmentation: an overview of the common afflictions.
Cayce KA, McMichael AJ, Feldman SR.
Dermatol Nurs. 2004 Oct;16(5):401-6, 413-6; quiz 417. Review.
Topical agents used in the management of hyperpigmentation.
Halder RM, Richards GM.
Skin Therapy Lett. 2004 Jun-Jul;9(6):1-3. Review.
Optimal management of recalcitrant disorders of hyperpigmentation in dark-skinned patients.
Stratigos AJ, Katsambas AD.
Am J Clin Dermatol. 2004;5(3):161-8. Review.
Management of dyschromias in ethnic skin.
Halder RM, Richards GM.
Dermatol Ther. 2004;17(2):151-7. Review.
Common hyperpigmentation disorders in adults: Part II. Melanoma, seborrheic keratoses, acanthosis nigricans, melasma, diabetic dermopathy, tinea versicolor, and postinflammatory hyperpigmentation.
Stulberg DL, Clark N, Tovey D.
Am Fam Physician. 2003 Nov 15;68(10):1963-8. Review.
Disorders of hyperpigmentation.
Pandya AG, Guevara IL.
Dermatol Clin. 2000 Jan;18(1):91-8, ix. Review.
Regional dermatoses in the African. Part I. Facial hypermelanosis.
Olumide YM, Odunowo BD, Odiase AO.
Int J Dermatol. 1991 Mar;30(3):186-9. Review.
Postinflammatory hyperpigmentation

Postinflammatory hyperpigmentation in irritant dermatitis. © DermNetNZ

Postinflammatory hyperpigmentation in inflamed cyst. © DermNetNZ
Efficacy and Best Mode of Delivery for Tranexamic Acid in Post-Inflammatory Hyperpigmentation: A Systematic Review. Alsharif SH, Alghamdi AS, Alwayel ZA, Alaklabi SN, Alyamani NA, Sabsabee MA, Bu Izran DAA, Alajlan AM. Clin Cosmet Investig Dermatol. 2022 Dec 28;15:2873-2882. doi: 10.2147/CCID.S394889. PMID: 36597522; PMCID: PMC9805721. Systematic Review.
Topical treatment for postinflammatory hyperpigmentation: a systematic review. Tan MG, Kim WB, Jo CE, Nabieva K, Kirshen C, Ortiz AE. J Dermatolog Treat. 2022 Aug;33(5):2518-2526. doi: 10.1080/09546634.2021.1981814. Epub 2021 Sep 27. PMID: 34525885. Systematic Review.
Excoriation (skin-picking) disorder among adolescents and young adults with acne-induced postinflammatory hyperpigmentation and scars. Ekore RI, Ekore JO. Int J Dermatol. 2021 Dec;60(12):1488-1493. doi: 10.1111/ijd.15587. Epub 2021 Apr 16. PMID: 33860536 Review.
Effects of Topical Retinoids on Acne and Post-inflammatory Hyperpigmentation in Patients with Skin of Color: A Clinical Review and Implications for Practice. Callender VD, Baldwin H, Cook-Bolden FE, Alexis AF, Stein Gold L, Guenin E. Am J Clin Dermatol. 2021 Nov 9. doi: 10.1007/s40257-021-00643-2. Online ahead of print. PMID: 34751927
Prophylaxis of Post-Inflammatory Hyperpigmentation From Energy-Based Device Treatments: A Review [Formula: see text]. Wong ITY, Richer V. J Cutan Med Surg. 2021 Jan-Feb;25(1):77-86. doi: 10.1177/1203475420957633. Epub 2020 Sep 15. PMID: 32929988 Review.
The Pathogenesis and Management of Acne-Induced Post-inflammatory Hyperpigmentation. Elbuluk N, Grimes P, Chien A, Hamzavi I, Alexis A, Taylor S, Gonzalez N, Weiss J, Desai SR, Kang S. Am J Clin Dermatol. 2021 Sep 1. doi: 10.1007/s40257-021-00633-4. Online ahead of print. PMID: 34468934 Review.
Dermoscopy of acquired pigmentary disorders: a comprehensive review. Krueger L, Saizan A, Stein JA, Elbuluk N. Int J Dermatol. 2021 Jul 7. doi: 10.1111/ijd.15741. Online ahead of print. PMID: 34235719 Review.
Topical treatment strategies to manipulate human skin pigmentation. Rachmin I, Ostrowski SM, Weng QY, Fisher DE. Adv Drug Deliv Rev. 2020 Jan 1;153:65-71. doi: 10.1016/j.addr.2020.02.002. Epub 2020 Feb 21. PMID: 32092380 Free PMC article.
Topical treatment for postinflammatory hyperpigmentation: a systematic review. Tan MG, Kim WB, Jo CE, Nabieva K, Kirshen C, Ortiz AE. J Dermatolog Treat. 2021 Sep 27:1-9. doi: 10.1080/09546634.2021.1981814. Online ahead of print. PMID: 34525885
Post-Inflammatory Hyperpigmentation: A Review of Treatment Strategies. Shenoy A, Madan R. J Drugs Dermatol. 2020 Aug 1;19(8):763-768. doi: 10.36849/JDD.2020.4887. PMID: 32845587 Review.
Laser treatments for postinflammatory hyperpigmentation: A systematic review.
Agbai O, Hamzavi I, Jagdeo J.
JAMA Dermatol. 2016 Dec 14. doi: 10.1001/jamadermatol.2016.4399. [Epub ahead of print]. Systematic review.
Post-inflammatory hyperpigmentation: A review of treatment strategies.
Shenoy A, Madan R.
J Drugs Dermatol. 2020 Aug 1;19(8):763-768. doi: 10.36849/JDD.2020.4887. Review.
The role of sunscreen in melasma and postinflammatory hyperpigmentation.
Fatima S, Braunberger T, Mohammad TF, Kohli I, Hamzavi IH.
Indian J Dermatol. 2020 Jan-Feb;65(1):5-10. doi: 10.4103/ijd.IJD_295_18. Review.
Therapeutic insights in melasma and hyperpigmentation management.
Huerth KA, Hassan S, Callender VD.
J Drugs Dermatol. 2019 Aug 1;18(8):718-729. Review.
What's new in pigmentary disorders.
Zubair R, Lyons AB, Vellaichamy G, Peacock A, Hamzavi I.
Dermatol Clin. 2019 Apr;37(2):175-181. doi: 10.1016/j.det.2018.12.008. Epub 2019 Feb 16. Review.
Hyperpigmentation disorders in Hispanic population in the United States.
Rendon MI.
J Drugs Dermatol. 2019 Mar 1;18(3):s112-114. Review.
Postinflammatory hyperpigmentation: Epidemiology, clinical presentation, pathogenesis and treatment.
Kaufman BP, Aman T, Alexis AF.
Am J Clin Dermatol. 2017 Dec 8. doi: 10.1007/s40257-017-0333-6. [Epub ahead of print] Review.
Postinflammatory hyperpigmentation: A comprehensive overview: Epidemiology, pathogenesis, clinical presentation, and noninvasive assessment technique.
Silpa-Archa N, Kohli I, Chaowattanapanit S, Lim HW, Hamzavi I.
J Am Acad Dermatol. 2017 Oct;77(4):591-605. doi: 10.1016/j.jaad.2017.01.035. Review.
Postinflammatory hyperpigmentation: A comprehensive overview: Treatment options and prevention.
Chaowattanapanit S, Silpa-Archa N, Kohli I, Lim HW, Hamzavi I.
J Am Acad Dermatol. 2017 Oct;77(4):607-621. doi: 10.1016/j.jaad.2017.01.036. Review.
What devices to use or not use in skin of color.
Alam M.
Semin Cutan Med Surg. 2016 Dec;35(4):218-222. doi: 10.12788/j.sder.2016.061. Review.
Facial hyperpigmentation in skin of color: Special considerations and treatment.
Vashi NA, Wirya SA, Inyang M, Kundu RV.
Am J Clin Dermatol. 2016 Dec 9. [Epub ahead of print]. Review.
Skin hyperpigmentation in Indian population: Insights and best practice.
Nouveau S, Agrawal D, Kohli M, Bernerd F, Misra N, Nayak CS.Indian J Dermatol. 2016 Sep-Oct;61(5):487-95. doi: 10.4103/0019-5154.190103. Review.
Facial hyperpigmentation in darker skin types: Part 1.
Bala HR, Rodrigues M.
Dermatology in Practice. 2016 Autumn;22(3):79-82. Review.
Practice and educational gaps in abnormal pigmentation.
Mohammad TF, Hamzavi IH.
Dermatol Clin. 2016 Jul;34(3):291-301. doi: 10.1016/j.det.2016.02.005. Review.
Postinflammatory hyperpigmentation in patients with skin of color.
Shokeen D.
Cutis. 2016 Jan;97(1):E9-E11. Review.
Postinflammatory hyperpigmentation secondary to external insult: an overview of the quantitative analysis of pigmentation.
Lamel SA, Rahvar M, Maibach HI.
Cutan Ocul Toxicol. 2013 Mar;32(1):67-71. doi: 10.3109/15569527.2012.684419. Epub 2012 Jun 6. Review.
A focused review on acne-induced and aesthetic procedure-related postinflammatory hyperpigmentation in Asians.
Eimpunth S, Wanitphadeedecha R, Manuskiatti W.
J Eur Acad Dermatol Venereol. 2013 Jan;27 Suppl 1:7-18. doi: 10.1111/jdv.12050. Review.
Mechanisms underlying post-inflammatory hyperpigmentation: lessons from solar lentigo.
Cardinali G, Kovacs D, Picardo M.
Ann Dermatol Venereol. 2012 Dec;139 Suppl 4:S148-52. doi: 10.1016/S0151-9638(12)70127-8. Review.
Hydroquinone therapy for post-inflammatory hyperpigmentation secondary to acne: not just prescribable by dermatologists.
Chandra M, Levitt J, Pensabene CA.
Acta Derm Venereol. 2012 May;92(3):232-5. doi: 10.2340/00015555-1225. Review.
Lasers for treatment of melasma and post-inflammatory hyperpigmentation.
Arora P, Sarkar R, Garg VK, Arya L.
J Cutan Aesthet Surg. 2012 Apr;5(2):93-103. doi: 10.4103/0974-2077.99436. Review.
Postinflammatory hyperpigmentation: etiologic and therapeutic considerations.
Callender VD, St Surin-Lord S, Davis EC, Maclin M.
Am J Clin Dermatol. 2011 Apr 1;12(2):87-99. doi: 10.2165/11536930-000000000-00000. Review.
Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color.
Davis EC, Callender VD.
J Clin Aesthet Dermatol. 2010 Jul;3(7):20-31. Review.
Postinflammatory hyperpigmentation.
Taylor S, Grimes P, Lim J, Im S, Lui H.
J Cutan Med Surg. 2009 Jul-Aug;13(4):183-91. Review.
Topical treatments for melasma and postinflammatory hyperpigmentation.
Lynde CB, Kraft JN, Lynde CW.
Skin Therapy Lett. 2006 Nov;11(9):1-6. Review.
Postinflammatory hyperpigmentation: evolving combination treatment strategies.
Taylor SC, Burgess CM, Callender VD, Fu J, Rendon MI, Roberts WE, Shalita AR.
Cutis. 2006 Aug;78(2 Suppl 2):6-19. Review.
Postinflammatory hyperpigmentation: a common but troubling condition.
Lacz NL, Vafaie J, Kihiczak NI, Schwartz RA.
Int J Dermatol. 2004 May;43(5):362-5. Review.
Postinflammatory hyperpigmentation.
Epstein JH.
Clin Dermatol. 1989 Apr-Jun;7(2):55-65. Review.
Naevus of Ota & Ito
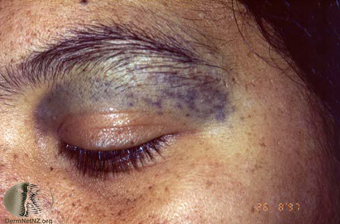
Naevus of Ota. © DermNetNZ

Naevus of Ito. © DermNetNZ
Melanoma in the setting of nevus of Ota: a review for dermatologists. Williams NM, Gurnani P, Labib A, Nuesi R, Nouri K. Int J Dermatol. 2021 May;60(5):523-532. doi: 10.1111/ijd.15135. Epub 2020 Aug 17. PMID: 32808287 Review.
Periorbital Discolouration Diagnosis and Treatment: Evidence-Based Review. Pissaridou MK, Ghanem A, Lowe N. J Cosmet Laser Ther. 2020 Nov 16;22(6-8):217-225. doi: 10.1080/14764172.2021.1899238. Epub 2021 Jun 3. PMID: 34078228 Review.
Comparing the efficacy and safety of Q-switched and picosecond lasers in the treatment of nevus of Ota: a systematic review and meta-analysis.
Williams NM, Gurnani P, Long J, Reynolds J, Pan Y, Suzuki T, Alhetheli GI, Nouri K.
Lasers Med Sci. 2020 Aug 24. doi: 10.1007/s10103-020-03125-9. Online ahead of print. Systematic review.
Comparison of clinical efficacy and complications between Q-switched alexandrite laser and Q-switched Nd:YAG laser on nevus of Ota: a systematic review and meta-analysis.
Yu P, Yu N, Diao W, Yang X, Feng Y, Qi Z.
Lasers Med Sci. 2016 Apr;31(3):581-91. doi: 10.1007/s10103-016-1885-z. Epub 2016 Feb 9. Systematic review.
[Treatment of nevus of Ota and Ito and epidermal nevus syndrome].
Badawi A, Osman MA, Kassab AN.
Hautarzt. 2020 Dec;71(12):926-931. doi: 10.1007/s00105-020-04710-3. German. Review.
Melanoma in the setting of nevus of Ota: a review for dermatologists.
Williams NM, Gurnani P, Labib A, Nuesi R, Nouri K.
Int J Dermatol. 2020 Aug 17. doi: 10.1111/ijd.15135. Online ahead of print. Review.
Laser treatment of hyperpigmented lesions: position statement of the European Society of Laser in Dermatology.
Passeron T, Genedy R, Salah L, Fusade T, Kositratna G, Laubach HJ, Marini L, Badawi A.
J Eur Acad Dermatol Venereol. 2019 Mar 14. doi: 10.1111/jdv.15497. [Epub ahead of print]. Review.
Variables that predict response of nevus of ota to lasers.
Rani S, Sardana K.
J Cosmet Dermatol. 2019 Feb 5. doi: 10.1111/jocd.12875. [Epub ahead of print]. Review.
Dermal melanocytosis and associated disorders.
Franceschini D, Dinulos JG.
Curr Opin Pediatr. 2015 Aug;27(4):480-5. doi: 10.1097/MOP.0000000000000247. Review.
Three cases of symmetrical nevus of Ota and a brief literature review.
Yang T, Jiang X.
Int J Dermatol. 2016 Feb 17. doi: 10.1111/ijd.13087. [Epub ahead of print]. Review. No abstract available.
Lasers and nevus of Ota: a comprehensive review.
Shah VV, Bray FN, Aldahan AS, Mlacker S, Nouri K.
Lasers Med Sci. 2016 Jan;31(1):179-85. doi: 10.1007/s10103-015-1834-2. Epub 2015 Nov 12. Review.
Melanoma arising in a nevus of Ito: novel genetic mutations and a review of the literature on cutaneous malignant transformation of dermal melanocytosis.
Tse JY, Walls BE, Pomerantz H, Yoon CH, Buchbinder EI, Werchniak AE, Dong F, Lian CG, Granter SR.
J Cutan Pathol. 2015 Aug 11. doi: 10.1111/cup.12568. [Epub ahead of print]. Review.
Acquired bilateral nevus of Ota-like macules (Hori nevus): etiologic and therapeutic considerations.
Park JM, Tsao H, Tsao S.
J Am Acad Dermatol. 2009 Jul;61(1):88-93. doi: 10.1016/j.jaad.2008.10.054. Review.
Nevus of Ota in children.
Sinha S, Cohen PJ, Schwartz RA.
Cutis. 2008 Jul;82(1):25-9. Review.
Late-onset Ito's nevus: an uncommon acquired dermal melanocytosis.
Mataix J, López N, Haro R, González E, Angulo J, Requena L.
J Cutan Pathol. 2007 Aug;34(8):640-3. Review.
Nevus of Ota: clinical aspects and management.
Chan HH, Kono T.
Skinmed. 2003 Mar-Apr;2(2):89-96; quiz 97-8. Review.
Are these pigmentary changes only cosmetic? Oculodermal melanocytosis (nevus of Ota).
Mishriki YY.
Postgrad Med. 2001 Dec;110(6):43-6. Review.
Nevus of Ota.
Tyndel FJ, Davidson GS, Bilbao JM.
Neurology. 1994 Mar;44(3 Pt 1):586. Review.
Exogenous ochronosis

Ochronosis. © Waikato District Health Board
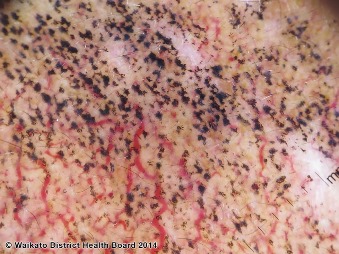
Ochronosis. © Waikato District Health Board
Dogliotti and Phillips classifications are unsuitable for grading the histopathological findings of exogenous ochronosis. Ramia de Cap M, Parisi X, Tahan SR. J Cutan Pathol. 2021 Dec 16. doi: 10.1111/cup.14189. Online ahead of print. PMID: 34918365
Exogenous ochronosis associated with hydroquinone: a systematic review. Ishack S, Lipner SR. Int J Dermatol. 2021 Sep 6. doi: 10.1111/ijd.15878. Online ahead of print. PMID: 34486734 Review.
Vashi NA, Wirya SA, Inyang M, Kundu RV.
Am J Clin Dermatol. 2016 Dec 9. [Epub ahead of print]. Review.
Exogenous ochronosis.
Bhattar PA, Zawar VP, Godse KV, Patil SP, Nadkarni NJ, Gautam MM.
Indian J Dermatol. 2015 Nov-Dec;60(6):537-43. doi: 10.4103/0019-5154.169122. Review.
Exogenous ochronosis: a comprehensive review of the diagnosis, epidemiology, causes, and treatments.
Simmons BJ, Griffith RD, Bray FN, Falto-Aizpurua LA, Nouri K.
Am J Clin Dermatol. 2015 Jun;16(3):205-12. doi: 10.1007/s40257-015-0126-8. Review.
Exogenous ochronosis. An update on clinical features, causative agents and treatment options.
Levin CY, Maibach H.
Am J Clin Dermatol. 2001;2(4):213-7. Review.
Periorbital hyperpigmentation
Treatments of periorbital hyperpigmentation: A systematic review.
Michelle L, Pouldar Foulad D, Ekelem C, Saedi N, Mesinkovska NA.
Dermatol Surg. 2020 Jul 31. doi: 10.1097/DSS.0000000000002484. Online ahead of print. Systematic review.
Facial hyperpigmentation in skin of color: Special considerations and treatment.
Vashi NA, Wirya SA, Inyang M, Kundu RV.
Am J Clin Dermatol. 2016 Dec 9. [Epub ahead of print]. Review.
Skin hyperpigmentation in Indian population: Insights and best practice.
Nouveau S, Agrawal D, Kohli M, Bernerd F, Misra N, Nayak CS.Indian J Dermatol. 2016 Sep-Oct;61(5):487-95. doi: 10.4103/0019-5154.190103. Review.
Infraorbital dark circles: A review of the pathogenesis, evaluation and treatment.
Vrcek I, Ozgur O, Nakra T.
J Cutan Aesthet Surg. 2016 Apr-Jun;9(2):65-72. doi: 10.4103/0974-2077.184046. Review.
Periorbital hyperpigmentation: A comprehensive review.
Sarkar R, Ranjan R, Garg S, Garg VK, Sonthalia S, Bansal S.
J Clin Aesthet Dermatol. 2016 Jan;9(1):49-55. Review.
Dark circles: etiology and management options.
Friedmann DP, Goldman MP.
Clin Plast Surg. 2015 Jan;42(1):33-50. doi: 10.1016/j.cps.2014.08.007. Review.
Periorbital hyperpigmentation: review of etiology, medical evaluation, and aesthetic treatment.
Roberts WE.
J Drugs Dermatol. 2014 Apr;13(4):472-82. Review.
Periocular hyperpigmentation: a review of etiology and current treatment options.
Alsaad SM, Mikhail M.
J Drugs Dermatol. 2013 Feb;12(2):154-7. Review.
Infraorbital dark circles: definition, causes, and treatment options.
Roh MR, Chung KY.
Dermatol Surg. 2009 Aug;35(8):1163-71. doi: 10.1111/j.1524-4725.2009.01213.x. Epub 2009 May 15. Review.
What causes dark circles under the eyes?
Freitag FM, Cestari TF.
J Cosmet Dermatol. 2007 Sep;6(3):211-5. Review.
Back to index page