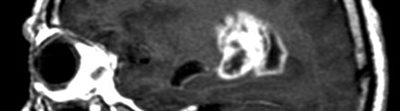
Brain scan
A polymer originally designed to help mend broken bones could be successful in delivering chemotherapy drugs directly to the brains of patients suffering from brain tumours, researchers at The University of Nottingham have discovered.
Their study, published in the journal PLOS ONE, shows that the biomaterial can be easily applied to the cavity created following brain cancer surgery and used to release chemotherapy drugs over several weeks.
The targeted nature of the therapy could also reduce the toxic effects of chemotherapy drugs on healthy parts of the body, potentially reducing the debilitating side-effects that many patients experience after cancer treatment.
Patient survival
Dr Ruman Rahman, of the University’s Children’s Brain Tumour Research Centre (CBTRC), who led the study, said: “Our system is an innovative method of drug delivery for the treatment of brain tumours and is intended to be administered immediately after surgery by the operating neurosurgeon.
“Ultimately, this method of drug delivery, in combination with existing therapies, may result in more effective treatment of brain tumours, prolonged patient survival and reduced morbidity.”
Brain tumours are the major cause of cancer-related death in children and adults up to the age of 40. Most relapses occur when surgeons are unable to remove all of the cancerous cells during surgery – something which can be particularly challenging in very young children and babies and by the very nature of a type of adult brain cancer called glioblastoma.
Although alternative systems for delivery of drugs directly to the brain have been developed, they are used infrequently because their success has been limited. This new drug delivery system is the first that can be moulded to the shape of the brain tumour cavity and the first to deliver several different drugs over a clinically meaningful period of time.
The Nottingham polymer formulation is made from two types of micro-particles called PLGA and PEG and has been developed and patented by leading tissue engineer Professor Kevin Shakesheff, based in the University’s School of Pharmacy. A powder at room temperature, it can be mixed to a toothpaste-like consistency with the addition of water.
Follow this link to see the full story
Posted on Wednesday 13th November 2013